Reducing Inflammation Could Decrease Obesity
By: Crystal Price
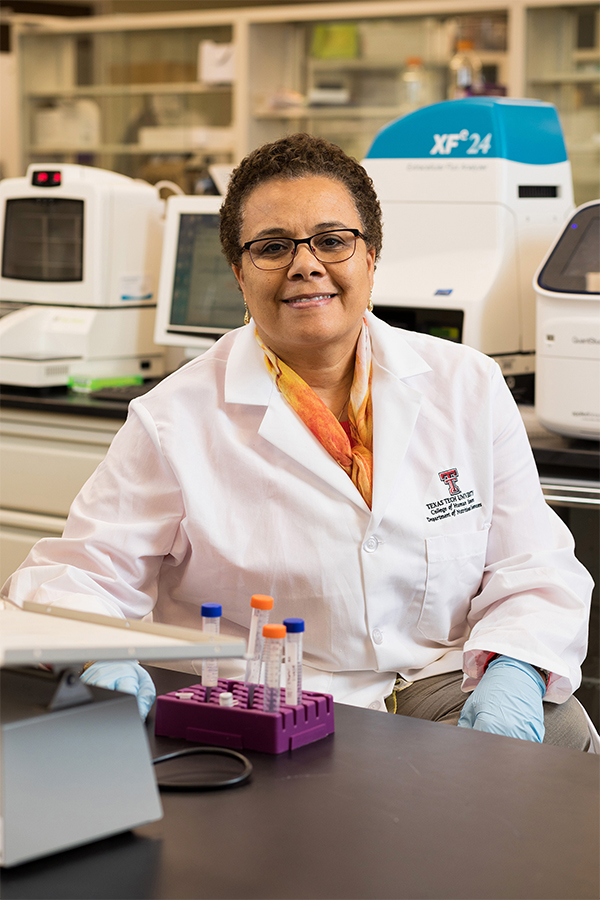
In 2013, Naima Moustaid-Moussa, professor of nutritional science in the College of Human Sciences and adjunct professor in Plant and Soil Science, began her journey at Texas Tech by starting the Obesity Research Cluster (ORC). Due to Moustaid-Moussa's continued dedication, leadership and hard work in obesity research, the ORC was officially upgraded to the Obesity Research Institute (ORI) in March.
Moustaid-Moussa has grown the ORI into an interdisciplinary collaboration involving faculty in many diverse fields. “Factors such as strengthening the research base through faculty and student collaborations, staying engaged with the local community, and attaining more visibility through inviting external expert guest speakers and ORC- sponsored workshops at national conferences, and research funding have really propelled ORI to the next level,” Moustaid-Moussa says.
Of course, it is also the hard work Moustaid-Moussa and her team have provided in the realm of obesity research and the new ways of thinking about the disease. Currently, Moustaid-Moussa and the ORI are focused on finding ways to decrease negative effects in the body from obesity.
ORI members conduct research ranging from basic science to clinical studies all the way to community-based nutrition research.
Obesity is a disorder involving excessive body fat, or adipose tissue, that increases the risk of health problems. Adipose tissue exists in two forms in the human body. One is white adipose tissue (WAT), also known as bad fat, and the other is brown adipose tissue (BAT), or good fat.
Moustaid-Moussa asks two important questions to learn more about the role of adipose tissue in obesity: What is the role of fat tissue, and what causes fat cells to expand?
“Many times,” Moustaid-Moussa says, “the body recognizes this excess fat as an attack on the immune system thus triggering an inflammatory response. This can be problematic for many reasons including glucose levels rising due to increased production of glucose by the liver as well as insulin resistance, which is a reduced ability of insulin response within the body.”
The fat tissue itself starts to produce hormones, such as leptin, which controls appetite and angiotensine II, which raises blood pressure, that make the fat tissue an important and active endocrine organ. Moustaid-Moussa is actively working to discover how to stop adipose tissue from producing excessive amounts of these hormones.
Currently, mice are the test subjects for Moustaid-Moussa's research in the ORI. Some are being tested with pharmacological treatments and others with diet or through genetic engineering. Most animal models showed that a high fat diet increased obesity, insulin resistance, and inflammation.
Moustaid-Moussa said obesity can occur in an otherwise healthy person as well as one that is overweight. To reduce the negative effects of obesity, targeting any inflammation is key. One dietary compound that Moustaid-Moussa has been using is Omega-3 fatty acids. These are found in fish and fish oil and have been linked to reduced inflammation. In many ways, they work just like non-steroidal anti-inflammatory drugs such as aspirin or ibuprofen.
Once Moustaid-Moussa and her team started testing fish oil on mice, they began to see weight loss and inflammation subsiding. They also discovered that when the inflammation was blocked, the symptoms of diabetes decreased. Another collateral benefit of fish oil in these mice was activation of brown fat, which Moustaid-Moussa and Latha Ramalingam, a research assistant professor in the Department of Nutritional Sciences, are investigating through funding from the National Institutes of Health's (NIH) National Center for Complementary and Integrative Health (NCCIH).
Most recently, through supplemental funding from the NIH National Institute of Aging (NIA), Moustaid-Moussa collaborated with Breanna Harris, a research assistant professor in the Department of Biological Sciences, and extended this line of research to test whether fish oil protects against Alzheimer's disease. The total funding from NIH for this research amounted to $799,000.
Moustaid-Moussa then decided to add tart cherry, which contains a bioactive compound anthocyanin, to the fish oil. “There are added benefits to consuming both Omega-3 fatty acids and tart cherries,” Moustaid-Moussa said, “the reason for choosing these two dietary compounds is that we, and other scientists, have shown that individually they greatly reduce inflammation and fat accumulation that accompanies obesity, both in animal and cell culture models.”
Moustaid-Moussa says both tart cherry and Omega-3 block inflammation, but Omega-3 also helps rejuvenate BAT, which could aid in decreasing obesity. “The individual protective effects of Omega-3 fatty acids and tart cherry are amplified when combined, even at lower amounts than when tested individually,” Moustaid-Moussa said.
Since Moustaid-Moussa and her team have seen various results from Omega-3 and tart cherry, new questions are being asked such as how fat cells and immune cell inflammation affects other organs and what role Omega-3 and tart cherry could play in decreasing these effects.
With new funding of $500,000 from the United States Department of Agriculture (USDA) National Institute of Food and Agriculture (NIFA) for the 2019 Agriculture and Food Research Initiative (AFRI), Moustaid-Moussa's team, consisting of Kate Larson, Latha Ramalingam, Jung Han Kim, and John Dawson, will continue to delve into the use of Omega-3 and tart cherry.
The research Moustaid-Moussa conducts could be beneficial to cancer treatment as well. Since Omega-3 produces protective effects in the body, inflammation within cancer cells could be reduced. Currently, this has only been tested on isolated cells, but testing on mice could happen before long.
More of this type of research is necessary to understand the benefits of a diverse diet for obesity and inflammation and the positive impacts gained over time within the human body. Along with Moustaid-Moussa's work, other members of ORI have received funding from USDA, NIH, AHA, and other national and international agencies to study obesity.
“We are excited to see how the ORI will grow and thrive in the future,” Moustaid-Moussa said with a grin on her face. ORI will continue fostering and leading multidisciplinary research collaborations within and outside Texas Tech, with the ultimate goal of increasing funding, visibility, and recognition of obesity research at Texas Tech.
Discoveries
-
Address
Texas Tech University, 2500 Broadway, Box 41075 Lubbock, TX 79409 -
Phone
806.742.3905 -
Email
vpr.communications@ttu.edu
