Dr. Harvinder Singh Gill Awarded $1.8M Grant from the National Institutes of Health
By Rachel Dolle
 Prevalence of allergic disease has continued to rise worldwide for more than 50 years.
An estimated 40 percent of the population is sensitized, i.e., have Immunoglobulin
E (IgE) antibodies to foreign proteins in the environment. (IgE are antibodies produced
by the immune system. If you have an allergy, your immune system overreacts to an
allergen by producing IgE antibodies. These antibodies travel to cells that release
chemicals, causing an allergic reaction). More worrisome, 40%-50% of school-going
children worldwide are getting sensitized to one or more allergens. For example, about
6 million children in the United States suffer from food allergies against peanut,
milk, egg, shellfish etc. Other forms of sensitizing allergens can include a multitude
of foreign proteins derived from pollens, insects, dust mites and vegetation, which
can manifest as different diseases including allergic rhinitis (hay fever), sinusitis,
asthma and skin reactions. One might even consider allergy as the emerging epidemic
of the industrialized world.
Prevalence of allergic disease has continued to rise worldwide for more than 50 years.
An estimated 40 percent of the population is sensitized, i.e., have Immunoglobulin
E (IgE) antibodies to foreign proteins in the environment. (IgE are antibodies produced
by the immune system. If you have an allergy, your immune system overreacts to an
allergen by producing IgE antibodies. These antibodies travel to cells that release
chemicals, causing an allergic reaction). More worrisome, 40%-50% of school-going
children worldwide are getting sensitized to one or more allergens. For example, about
6 million children in the United States suffer from food allergies against peanut,
milk, egg, shellfish etc. Other forms of sensitizing allergens can include a multitude
of foreign proteins derived from pollens, insects, dust mites and vegetation, which
can manifest as different diseases including allergic rhinitis (hay fever), sinusitis,
asthma and skin reactions. One might even consider allergy as the emerging epidemic
of the industrialized world.
Currently, 'Allergen-specific immunotherapy (ASI)' is the only disease-modifying treatment available, which can desensitize humans to their allergen. Subcutaneous immunotherapy, also known as allergy-shots, have been the standard for performing ASI. It involves repeated injections of the allergen under the patient's skin to reorient their abnormal allergy-causing immune responses. Conventional needle-based allergy-shots have several drawbacks, including the need for repeated allergen injections over multiple years, the need to be in a clinic to receive the treatment, and a risk of life-threatening systemic anaphylactic reaction (an allergic reaction that can occur quickly – as fast as within a couple of minutes of exposure to the allergen). Alternatively, sublingual immunotherapy, which involves holding the allergen under the tongue and either swallowing or spitting it out, has gained approval, although it involves the use of a much higher dose than the allergy-shots. New methods of allergy immunotherapy are being explored.
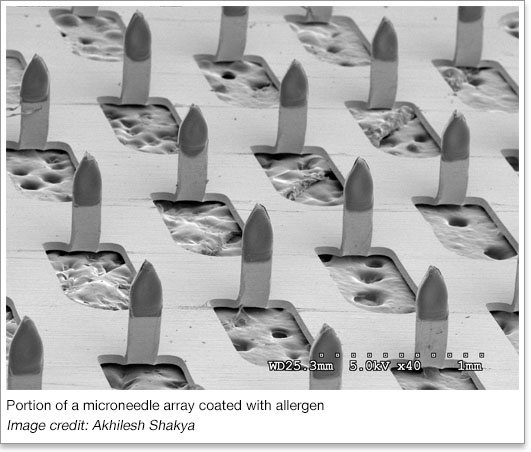
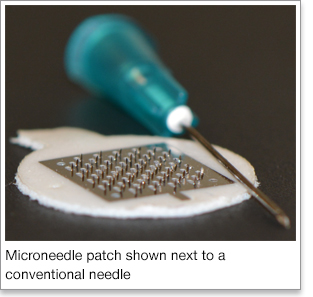 Dr. Harvinder Singh Gill, an associate professor of chemical engineering at Texas Tech University, has been
awarded a $1.8 million grant from the National Institutes of Health (NIH) to study
the use of microneedles for painless allergy immunotherapy. The goal of Gill's research
is to develop a novel minimally-invasive cutaneous immunotherapy (CIT) using allergen-coated
microneedles. Microneedles comprise of microscopic projections on a patch that can
be self-applied on the skin. Starting out as a thin sheet of stainless steel, the
microneedles are cut out of the steel and bent upward, resulting in a patch with a
flat surface containing approximately 57 needles. The microneedles can be coated with
the chosen allergen through a micro-precision coating device made specifically for
the coating process. The allergen is thereby effectively and efficiently applied only
to the microneedles themselves and not to the base of the stainless steel patch, minimizing
waste of expensive resources, and ensuring dose-consistency. Dosage amounts can also
be controlled, with the possibility of being able to use lower doses than necessary
with allergy-shots. This method could take the fear, pain, and inconvenience out of
allergy immunotherapy. Preliminary data show that microneedle-CIT is at least as
effective as allergy-shots. Gill's study will develop microneedles coated with allergens
and test their efficacy in comparison to the conventional needle-based allergy-shots.
Dr. Harvinder Singh Gill, an associate professor of chemical engineering at Texas Tech University, has been
awarded a $1.8 million grant from the National Institutes of Health (NIH) to study
the use of microneedles for painless allergy immunotherapy. The goal of Gill's research
is to develop a novel minimally-invasive cutaneous immunotherapy (CIT) using allergen-coated
microneedles. Microneedles comprise of microscopic projections on a patch that can
be self-applied on the skin. Starting out as a thin sheet of stainless steel, the
microneedles are cut out of the steel and bent upward, resulting in a patch with a
flat surface containing approximately 57 needles. The microneedles can be coated with
the chosen allergen through a micro-precision coating device made specifically for
the coating process. The allergen is thereby effectively and efficiently applied only
to the microneedles themselves and not to the base of the stainless steel patch, minimizing
waste of expensive resources, and ensuring dose-consistency. Dosage amounts can also
be controlled, with the possibility of being able to use lower doses than necessary
with allergy-shots. This method could take the fear, pain, and inconvenience out of
allergy immunotherapy. Preliminary data show that microneedle-CIT is at least as
effective as allergy-shots. Gill's study will develop microneedles coated with allergens
and test their efficacy in comparison to the conventional needle-based allergy-shots.
Gill's research will be conducted over a 5 year period. With success, these studies will provide data necessary to support further development of microneedles for painless allergy immunotherapy.
Edward E. Whitacre Jr. College of Engineering
-
Address
100 Engineering Center Box 43103 Lubbock, Texas 79409-3103 -
Phone
806.742.3451 -
Email
webmaster.coe@ttu.edu
